We need to stop giving suicide a silent treatment.
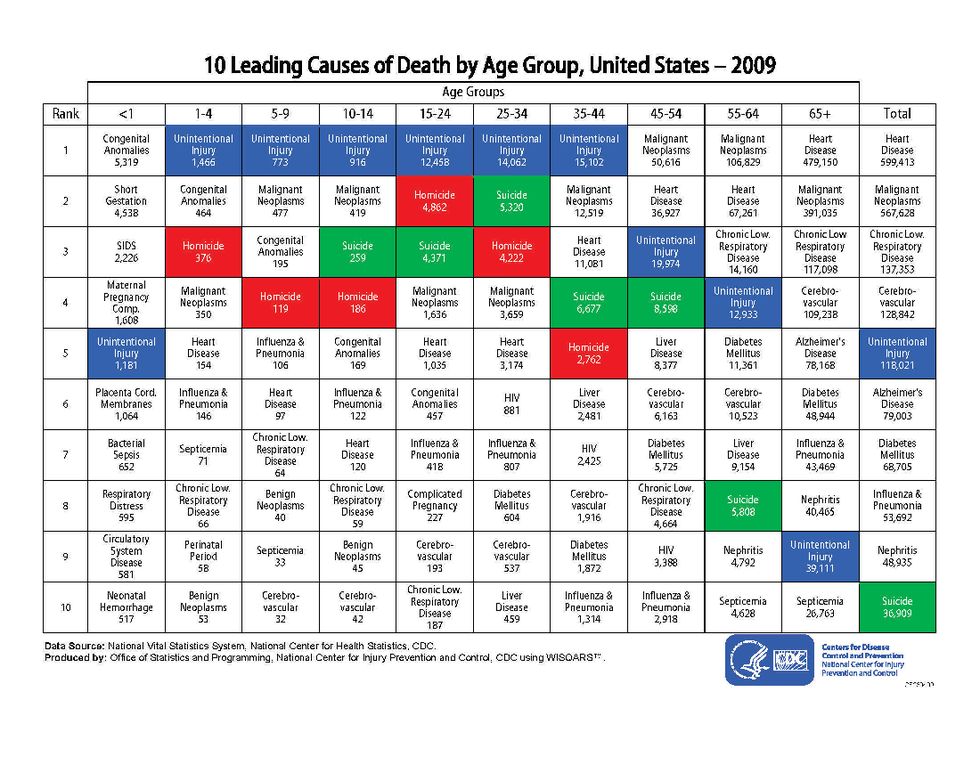
Suicide is the 10th leading cause of death for the general population in the United States, the 3rd leading cause of death in persons ages 10 to 24, and is often the least talked about. Suicide has culturally been painted as an "insensitive cry for attention", where people who struggle with suicidal ideation are seen as "weak" or "selfish."
(Provided by the CDC. Green is suicide, red is homicide, and blue is unintentional injury)
The stigma against suicide presents a barrier for those battling with these thoughts to reach out to necessary support. It's hard to ask for help when you feel like a burden for suffering, or when that feel as though your pain is not real. Asking for help becomes even more difficult when resources for support are at a deficit.
Offering professional support to those struggling with suicide comes with its own complexities. Treating patients who struggle with suicide raises both financial and emotional fears for many practitioners in the mental health field.
"The doctors I spoke with about this gave me different statistics on the number of mental-health professionals whose patients commit suicide. One says 51 percent of psychiatrists; another tells me it’s as high as 80 percent of all people who work in the mental-health field—including psychologists, social workers, etc. But the stigma of suicide is so strong that it’s often an issue left unspoken, even by doctors. Many psychiatrists refuse to treat chronically suicidal patients, not only because of the stigma that surrounds it even in their profession, but because suicide is the number-one cause of lawsuits brought against mental-health treatment providers."
Risk factors (American Foundation for Suicide Prevention)
- Mental health conditions
- Depression
- Anxiety
- Bipolar or other mood disorder
- Borderline personality disorder
- Antisocial personality disorder
- Conduct disorder
- Psychotic disorders or symptoms
- Substance abuse disorders
- Chronic health condition
- Chronic pain condition
- Environmental factors
- Stressful life events
- Divorce, death, job loss, etc.
- Prolonged stress factors
- Harassment, bullying, abuse, unemployment/financial instability, relationship issues, etc.
- Access to lethal means
- Exposure to another's suicide
- Stressful life events
- Historical factors
- Previous suicide attempts
- Family history of suicide attempts
Warning signs (Suicide Prevention Lifeline)
- Talking about wanting to die or kill one's self
- Looking for ways to kill one's self or accessing lethal means
- Talking about hopelessness or not having a reason to live
- Talking about feeling trapped or in "unbearable pain
- Talking about feeling like a burden
- Increased use of drugs and/or alcohol
- Anxious, agitated, or reckless behavior
- Sleeping too little or too much
- Withdrawing or feeling isolated
- Showing rage
- Seeking revenge
- Displaying mood swings
- Getting rid of one's belongings
How to help (NAMI)
- Remove weapons, stockpiled pills, or other lethal means
- Ask openly: "Are you having thoughts of suicide?"
- Ask openly: "Do you have a plan"
- Ask what you can do to help
- Don't argue or raise your voice
- Be gentle and sympathetic, especially if your loved one is having hallucinations
- Work to listen to their needs. Are they tired, hungry, angry, or feeling alone?
- Give them safe options.
- Keep checking in
- Bring them to a professional or emergency provider if they are in danger or expressing a serious plan
- Be an advocate, don't feed into myths
- Don't use guilt or claim that they're being selfish
- Educate yourself on their mental health issue and suicide as a whole
- Work on this safety plan with them
- Tell them that you care
If you are struggling, call the National Suicide Prevention Lifeline at:
1-800-273-8255
or utilize the Online Crisis Chat at: