Taking a conventional antidepressant medication (e.g. selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, tricyclic antidepressant, etc). to treat depression and various anxiety disorders is a personal choice.
As per Girish Subramanyan, some people are philosophically opposed to taking medications to treat conditions affecting their mental health. Others, perhaps out of despair, welcome anything that would alleviate their pain and suffering. As a practicing psychiatrist, I have treated both types of individuals.
Be that as it may, antidepressant medications are among a handful of evidence-based treatments for depression (Major Depressive Disorder) and the major anxiety disorders (Generalized Anxiety Disorder, Social Anxiety Disorder, Panic Disorder, Obsessive Compulsive Disorder and Post-Traumatic Stress Disorder). Other evidence-based treatments for Major Depressive Disorder include several forms of psychotherapy, including Cognitive Behavioral Therapy and Interpersonal Psychotherapy, exercise, phototherapy (light treatment), transcranial magnetic stimulation and electroconvulsive therapy. As well, there are several categories of antidepressant medications that are not mechanistically similar to reuptake inhibitor medications. These include monoamine oxidase inhibitors, ketamine and pramipexole, for example.
If you have experienced recurrent episodes of depression and have come to a point in your life where what you’ve done to help yourself on your own or psychotherapy have not been helpful, you may decide to pursue treatment with antidepressant medications. At this juncture, there are several important things to consider. The first is that if you respond to an antidepressant medication for your recurrent Major Depressive Disorder, you will likely have to take that medication indefinitely. The available evidence suggests that there is a high chance of relapse when antidepressants are withdrawn in recurrent Major Depressive Disorder.
However, the longer you take a reuptake inhibitor antidepressant medication, the harder it may be to come off it ever. Researchers in the field, such as Giovanni Fava and others, have hypothesized that chronic exposure to antidepressant medications results in neuroadaptive processes that, effectively, make the brain more likely to be depressed or anxious without the medication on board. They describe a mechanism called oppositional tolerance to explain this increased vulnerability. Effectively, the immediate physiological changes in the brain that result from antidepressant exposure result in compensatory changes in neuronal tissue via homeostatic mechanisms that attempt to minimize the physiological consequences of antidepressant exposure. Thus, you could say that while the antidepressant medication exerts its effect, the brain undergoes changes that push back against the effects of the antidepressant medication, leading to a state in which the brain is actually more vulnerable to depression and anxiety.
This hypothesis may explain one mechanism by which patients develop treatment-resistant mood and anxiety disorders: rapid discontinuation of the antidepressant medication after years of use. In this situation, Girish Subramanyan shares that, the antidepressant is withdrawn at a rate that does not allow the brain to fully undo the changes it made by being exposed to antidepressant in the first place. So, the pro-depressant, pro-anxiety state of the brain that occurs after chronic exposure to antidepressants is now unopposed by antidepressant medications and patients end up experiencing symptoms that are frequently more severe than the original symptoms which prompted them to seek medication treatment in the first place.
Certainly, in my practice of psychiatry, evaluating patients with treatment-resistant depressive disorders, some patients have given histories that strongly suggest that the development of treatment-resistance correlated with the period of time they discontinued an antidepressant medication they had been taking for years or were “cross-tapered” off their long-standing antidepressant medication and onto another antidepressant by a treatment provider.
The following website is replete with stories of individuals who have endured disastrous consequences from going off antidepressant medications too quickly:
https://www.survivingantidepressants.org/
Taken together, it’s a cautionary tale, certainly.
So, while going on antidepressant medications and staying on them are personal choices, I have advised patients over the years who wish to get off antidepressants to taper off as gradually as possible, in order to mitigate the risk of developing a protracted treatment-resistant mood or anxiety disorder. The general rule of thumb is a 10% dose reduction per month. Thus, if a patient is on 90 mg of duloxetine (Cymbalta) per day for her depression, she would decrease the dose to 81 mg/day for 1 month, then 72.9 mg/day the next month, then 65.6 mg/day the following month and so on and so forth. To achieve these non-commercially available intermediate doses, patients frequently have to use compounding pharmacies or oral suspensions to titrate off safely.
The timing of a depressive or anxious relapse after too rapid withdrawal from antidepressant medications can be either immediate or delayed (by many months, in some cases). Again, one characteristic of this type of relapse shared by Girish Subramanyan, is that it tends to usher in significantly more severe symptoms than the symptoms that accompanied the original condition for which the individual sought medication treatment.
While not all patients will develop a treatment-resistant mood or anxiety disorder after weaning off long-term antidepressant medication too rapidly, the unfortunate reality is that we are not yet able to predict who will. And the price that some individuals pay for doing so is much too great to approach the matter in a cavalier manner.
- theodysseynews Page 2 of 43 ›
- Automatic Gate Installation: What You Should Know? ›
- Stimulate Brain Health During Lockdown with John DenBoer ›
- I Love Being Home For Summer But I Miss My College Town ›
- Clueless Gifs That Accurately Describe A Sorority Girl ›
- Designing Home Doesn't Have To Be Hard: Read These 9 Tips ›




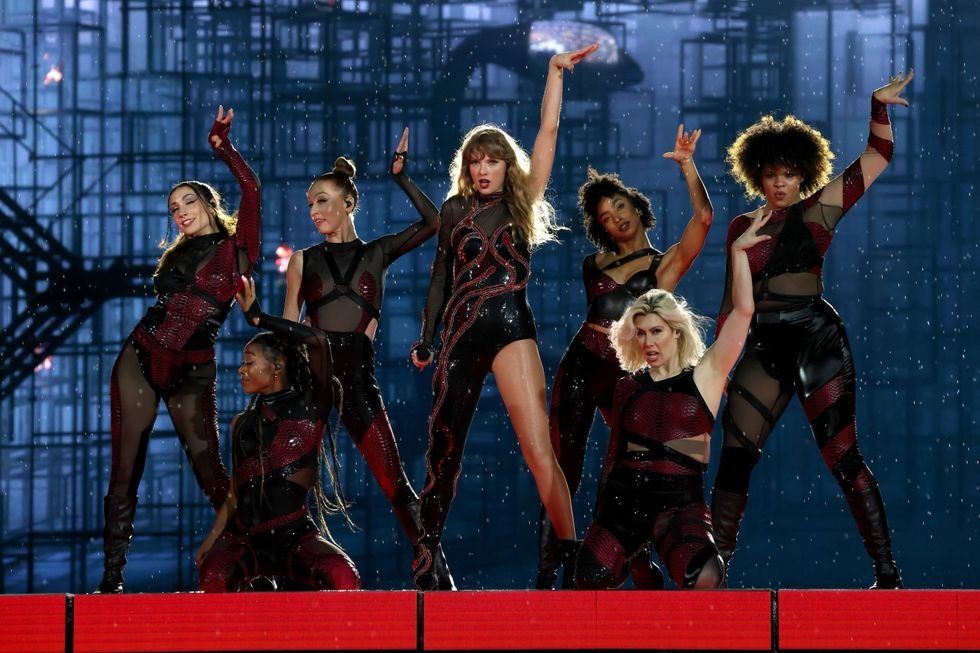 Energetic dance performance under the spotlight.
Energetic dance performance under the spotlight. Taylor Swift in a purple coat, captivating the crowd on stage.
Taylor Swift in a purple coat, captivating the crowd on stage. Taylor Swift shines on stage in a sparkling outfit and boots.
Taylor Swift shines on stage in a sparkling outfit and boots. Taylor Swift and Phoebe Bridgers sharing a joyful duet on stage.
Taylor Swift and Phoebe Bridgers sharing a joyful duet on stage.













