The modern U.S. health care system is highly effective and efficient at providing emergency medical care beyond that of any other country in the history of the world. However, the quality with which we provide some of the most basic of services has continued to decline over the past three decades. Simply put, the U.S. health care system has morphed into being more focused on productivity and technological advancement rather than quality patient care and cost containment.
Although a capitalistic structure for macroeconomic business models is undoubtedly the most effective method to generate revenue with the most consistent quality of product (as exemplified by the U.S. economy since the industrial revolution), it appears to be largely ineffective when applied to health care where the service provided directly affects human lives.
This conceptual dichotomy stems from a variety of aspects that collectively shape our perceptions of what's infecting the business of health care; each of which could be discussed ad nauseam. However, two that I'd like to touch on are that of physician involvement in the management of healthcare and the shock-wave of effects that were caused by the Medicare fee schedule.
U.S. healthcare is a $3.5 trillion industry that serves to provide 17.9% of the GDP. Integral to the delivery of that service are, undoubtedly, physicians and nurses as they are involved in its implementation on a daily basis. Why then, are the most experienced personnel in the industry almost entirely absent from the management of that system? Granted, physicians commonly go on to become hospital presidents, Chief Medical Officers, and into governmental positions, but I would argue that they should also be intricately involved in the more executive and financial positions within their individual organizations. Doing so would, not only, streamline health care delivery (as those who are providing the service are determining where resources should be allocated) but would also increase the level of trust that other health care workers have in management.
In fact, a 2011 survey revealed that 56% of physicians on hospital staffs didn't trust the administration as partners because of a lack of physician leadership. Additionally, in what seems to be an exponential increase in the rate of physician burnout, even this issue may be combated due to the executive doctor now having a vested interest and influence in the growth of his or her organization.
There are a few inherent problems with doing this, however. While physicians and nurses are the primary purveyors of health care, they often-times lack the necessary business skills to effectively manage a company or organization. Educational training programs that equip physicians to fill these roles are practically non-existent, with the exception of the Alliance for Physician Leadership at UT Southwestern. This need must then be met by alternative means such as earning a non-health care MBA or simply by fostering one's own managerial skills through acquiring non-clinical experience and the ever-important aspect of networking.
In order to expound on the impacts of the Medicare fee schedule (as it pertains to the decline in the quality of healthcare), a bit of a historical backdrop is necessary. Originally devised in 1985 by Harvard Economist, William Hsiao, was commissioned by the U.S. government to measure the exact amount of work involved in each of the tasks a doctor performs. He defined work as a function of time spent, mental effort and judgment, technical skill, physical effort, and stress. Overheads in training costs were also factored in. The team he assembled interviewed and surveyed physicians from approximately 24 different specialties, analyzing everything involved from 45 minutes of psychotherapy for a patient with panic attacks to a hysterectomy for a woman with cervical cancer. They determined that the hysterectomy takes 4.99 times as much work as the psychotherapy patient and used this method to evaluate thousands of other services. A relative value for everything doctors do was quantified. Congress then recommend a multiplier to convert the values into dollars and the new fee schedule was signed into law.
The fee schedule dictates which services a physician renders and governs a higher payout for more complex services than other [lesser] services. In 1992, Medicare began paying doctors accordingly and private insurance soon followed these same guidelines. Implemented as a top-down form of governance, the fee schedule is one of the primary reasons why our healthcare system has become so heavily reliant on output rather than patient care. By generating a standard that converts patient conditions to dollar signs, the focus was able to shift from patient care to generating revenue. Therefore, when the insurance companies adopted this schedule as a guideline for negotiations with physicians and hospitals, it effectively established all of health care as a business transaction instead of a service provided.
To understand what role government should play in our health care system and what the "end goal" should be, we must first understand what are the truths that we hold as self-evident and what it means for our rights to include that of "Life, Liberty, and the pursuit of Happiness." Doctor Robert Sade, in his paper on the interactions between politics and morality with that of medicine, explained that "The concept of medical care as the patient's right is immoral because it denies the most fundamental of all rights, that of a man to his own life and the freedom of action to support it.
Medical care is neither a right nor a privilege: it is a service that is provided by doctors and others to people who wish to purchase it." For a governing body to unilaterally dictate health care policy is to exalt their own reasoning and logic over that of the millions of individual minds associated with health care; be it physicians, patients, nurses, or policyholders. If we claim to desire a higher quality of patient-doctor relationships then we must keep the power of decision in the hands of those who are offering and consuming the service, namely, the doctor, nurse, and citizen.






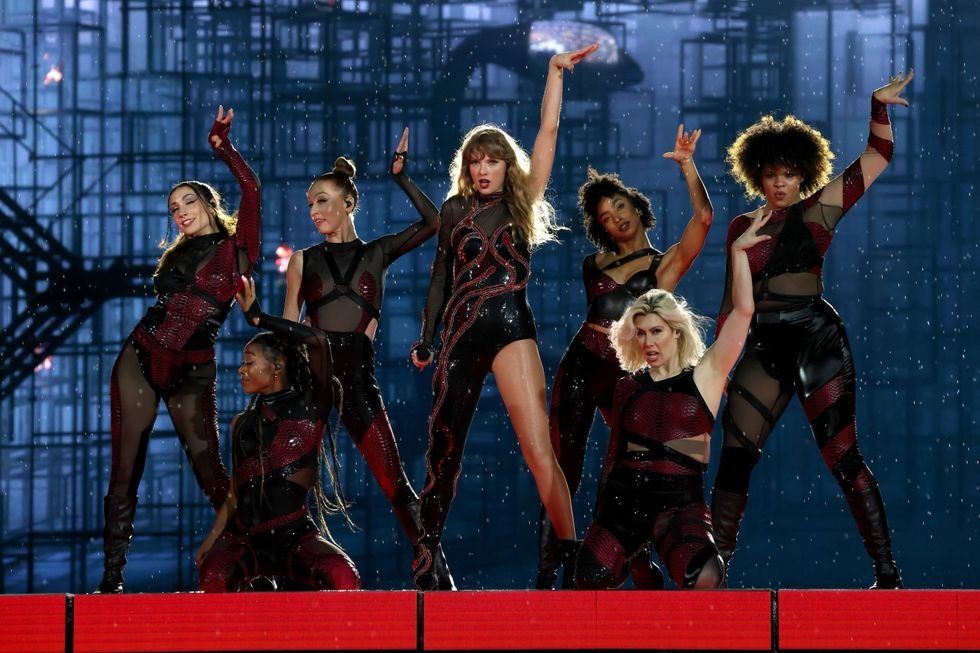 Energetic dance performance under the spotlight.
Energetic dance performance under the spotlight. Taylor Swift in a purple coat, captivating the crowd on stage.
Taylor Swift in a purple coat, captivating the crowd on stage. Taylor Swift shines on stage in a sparkling outfit and boots.
Taylor Swift shines on stage in a sparkling outfit and boots. Taylor Swift and Phoebe Bridgers sharing a joyful duet on stage.
Taylor Swift and Phoebe Bridgers sharing a joyful duet on stage.













