It was eight years ago when my symptoms started.
After a personal traumatic event, I went from being relatively healthy to a drastic manifestation of symptoms. Seemingly overnight I had diarrhea and gastrointestinal distress—the stomach distress was so bad that it sometimes doubled me over with sharp stabbing pain that even affected my ability to breathe. I had to actually leave social situations and dances because it would come on out of the blue and I'd be in agonizing pain.
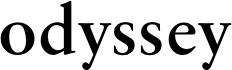
My parents were cautious of doctors and raised us kids to only go to the doctor in urgent circumstances, but I knew it wasn't normal to go from—well, normal—to diarrhea and stomach pain all the time. And it didn't go away. So months later, despite the childhood wariness of doctors, I set up doctors' appointments—and was met with an impatient male doctor who swept into the room, listened to my onset of symptoms, told me to "eat more fiber" and see if that would help, and swept out again in under five minutes.
So, I ate more fiber. I ate fibrous foods every day and took daily supplements to boot. After months of this doing nothing, I went back. The same doctor asked me questions about other symptoms—had I been running a fever? Found that this was related to dairy? Been eating too much fruit?—and then dismissed me with nothing, saying if the symptoms continued to come back, but for now, he wasn't worried.
After that, I scheduled an appointment with a different doctor, who told me my symptoms sound like IBS and that sucks for me because IBS isn't treatable and I'll just have to be careful about my diet, "suck it up" and deal with it. When I asked to be referred to a specialist he refused.
The third doctor I saw said the same thing: sounds like IBS, no, no need for you to see a specialist, sorry, you'll just have to deal with it. I asked if it could potentially be a food sensitivity or an allergy, because a lot of my symptoms seemed to fit with it being something diet-related, and was there someone I could see about that? Maybe testing for food sensitivities please?, especially gluten or lactose, since those seem to fit the symptoms?, and he said no, that's not it, it's just IBS. Eat fiber and figure out ways to get used to it.
When I disagreed with him and described the distress and pain I was in, he had the gall to tell me that I seemed very functional as I was continuing to work just fine and the pain couldn't be that bad if I hadn't been taking time off for it.
This turned me off of traditional doctors for years. I began going to natural health providers who genuinely listened and took a holistic and proactive approach to managing my symptoms. After being so dismissed by the traditional medical system, it was great to have people taking me seriously, saying, "No, that's not normal—you shouldn't have to live like that"—and doing something about it.
And I did all the things. You name it: if it was hippie and natural, I did it. Essential oils were the least of it. Humidifiers, colloidal silver, apple cider vinegar, hot lemon and honey and ginger, cloves of raw garlic, all sorts of vitamins and probiotics, etc.
I tried the FODMAP diet, sugar-free, gluten-free, only-protein-and-veggies, anti-inflammatory foods and spices, dark leafy greens every day, food tracking apps, etc. I ate so healthily that my little sister teased me about my lovership with kale and cheered whenever I ate ice cream or anything with sugar.
The natural health provider had me keep food diaries, drastically reduce sugar and carbs, and use $1,000s worth of supplements that genuinely eased some symptoms but didn't resolve things.
But I was getting worse. My immune system deteriorated: I came down with pneumonia, developed scar tissue in my lungs from it, was diagnosed with asthma, and began catching respiratory infections multiple times a year. I had insomnia and was exhausted all the time. During just one semester I came down with five separate fevers and four separate rounds of antibiotics that wiped out my immune system even more: I'd catch some other sort of cold or virus immediately when the round concluded. When I contracted a UTI, I opted for a shit-ton of cranberry juice and water and the pain of peeing for two weeks rather than go on antibiotics again. My coughs began turning into chronic bronchitis: I'd catch a cough in the fall and still be coughing up phlegm from that same cough in the summer.
I was working fulltime and going to school fulltime, so I worked while sick all the time. I couldn't afford to take off every day I felt miserable: I would have been working 2/3 less.
It was about the time I began dislocating my ribs by coughing* that I was like—okay. Time to go back to the doctors again.
*Oh yeah: did you know you could displace your ribs BY COUGHING?! I would have been happy to not know this for the rest of my life. I dislocated my fifth rib at the sternum on the right side of my body—and then a year and a half later, I dislocated/strained my 3rd and 4th on BOTH sides of my body, again from coughing.
The first time I went back with my symptoms, the male doctor I saw did the same dismissal thing. But my determination was newly renewed with my years-away hiatus and I'd done my research and prepared myself with determination to be my own advocate—I wouldn't take there's nothing we can do and no we won't refer you and eat more fiber for an answer.
I knew this wasn't normal for me. I knew this wasn't the best my body could be. I know they are the experts, but they aren't living in my body. This is significantly impacting my quality of life, and if there truly was "nothing to be done," then dammit, I wanted to make sure we exhausted every other option before I settled into a life of resignation.
And I knew enough now to know women are often taken less seriously by their doctors—nothing about those studies say that it's just male doctors who dismiss women, but by now I was tired of being dismissed exclusively by men.
So I left that office and explicitly searched for a female doctor, and found Dr. M.
And for the first time, I had a doctor who—when I described all the symptoms that had now been a part of my life for eight years (stomach pain, diarrhea, getting sick all the time, frequent respiratory illnesses)—and hesitantly concluded with, "And I don't think all these things are normal and things I should just get used to," Dr. M adamantly responded, "Absolutely not! We need to do something about this."
I felt like a shipwrecked sailor who finally saw sails on the horizon—after eight years of fighting a miserable battle against doctors on my own and just getting sicker and sicker and losing, it felt life-giving to have a knowledgeable doctor get in the ring with me too.
Dr. M began by ordering immediate tests for vitamin deficiencies. I asked about getting food testing and she promptly referred me. I also had researched several autoimmune disorders that seemed potentially relevant: I felt that the sudden onset of these particular symptoms and their lasting severity indicated a possible autoimmune source.
Getting in to see all these specialists took some time, and in the meantime, I asked if it was possible to be tested for a gluten intolerance sooner. Dr. M said, "Oh of course: that's a simple blood test that our labs can easily do." It came back: I was very intolerant of gluten. Without hesitation, she referred me to a gastroenterologist to schedule me for an endoscopy which confirmed: I had celiac disease, an autoimmune disease where the ingestion of gluten drastically damages the small intestine that had been triggered 8 years ago.

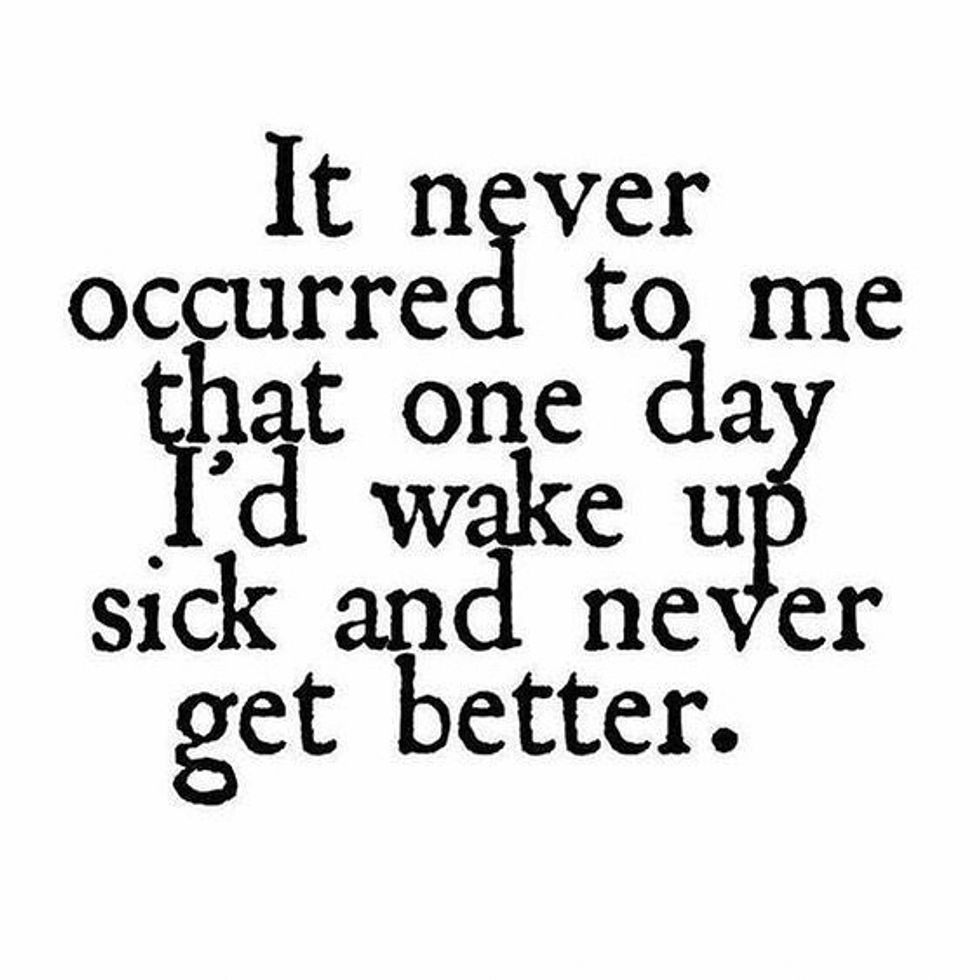
I had spent eight years in pain and getting sicker and sicker, all because those earlier doctors had waved a hand at my clear and dramatic symptoms and told me to "deal with it".
So much of the immune system rests in the gut—and mine had been destroyed for 8 years of being undiagnosed.
For 8 years I got progressively sicker, no matter how much effort I put into being healthy in the best way I knew how.
For 8 years I got more and more respiratory infections and chronic coughs, continuing to damage my lungs.
For 8 years I learned to adjust to constant internal distress and occasional pain: this was my life now, so I had to figure out how to live with it.
In those years, by the time I had gotten around to trying gluten-free diets in my self-attempts to heal myself, I didn't see any improvement (and therefore any reason to continue) because the damage to my intestines had been so significant that a month or two of being gluten-free wasn't enough to show results.
Now I have 5 ribs that have been dislocated or strained and healed poorly, as ribs do—ribs that pain me frequently and that might for the rest of my life. I have injuries to both knees that are worsened by how celiac affects bone health. I have autoimmune arthritis—100% caused by celiac. I've been anemic for years, because of celiac. (Before the celiac diagnosis I had gone on the carnivore diet as a last-ditch, extreme-diet way of trying to help my body heal: I'd heard great things of the carnivore diet healing gut-health for particular types of people. I ate nothing but meat, most of it red, for four weeks, and when I had my iron levels tested at the end of that time, I still tested as extremely anemic. If that doesn't tell you how little my body was absorbing nutrients, nothing will.)
And all it took to point in the celiac diagnosis direction was a simple, inexpensive, non-invasive blood test.
I'm sure you've seen the articles and studies that suggest women's health concerns are overlooked or dismissed by their doctors.
And perhaps it was mere coincidence that the doctor who ended up taking me seriously was a woman. After all, the studies show that women's symptoms are dismissed by doctors, not necessarily only male doctors.
But all the earlier doctors I had seen, who all downplayed and disregarded my symptoms—"eat more fiber," as if my autoimmune symptoms were my active fault—were male: and the first time I saw a female doctor, she took active steps to both listen to and uncover what was at the root of my ill health—and lo and behold, it did end up being a significant illness related to what I eat.
The diagnosis was so easy: the first step was a mere blood test.
If only that earlier doctor had listened to me asking to be tested for food sensitivities, this could have been discovered as soon as it started.
This was a sobering journey, and it's not done yet. I have several appointments with specialists whose specialties I can't even pronounce in the next month. But the celiac diagnosis was the biggest step toward becoming healthy again: now I know what's been causing so many of my problems and exacerbating almost all the others. And this journey definitely inspires an appreciation for the difficulty of finding a doctor who takes my concerns seriously and tackles my health issues side by side with me—and the gratefulness I feel for having persisted and finally found such a doctor, and my diagnosis.