I am a pharmacy student who spends several days a month working at a pharmacy that works closely with an addiction center. This morning, patients were lined up right at 9 A.M., when the pharmacy opens, to receive their Suboxone. Suboxone is a medication that is used to treat addiction and heroin is what we treat most commonly at our addiction center. Now you’re confused. How is heroin a part of the story about prescription painkillers?
A lot of the time these patients started out taking an opioid medication, such as oxycodone or morphine. They became addicted and in some cases the doctor keeps writing prescriptions for their patient. In other instances, the prescriptions stop, so the patient tries to fine something else to fuel their medical condition, addiction. Heroin hits the same receptors as opioids, so the users find a way to get heroin, which is becoming more accessible and it is cheaper. There is a statistic from an addiction center that states 4 out of 5 heroin addicts were previously on prescription painkillers. We do have patients that come in from the addiction center that are addicted to painkillers as well, but a lot of times, the painkillers end up leading to heroin.
So back to my morning, I had patients come in pick up a film as their daily dose. I give the patients the film, they slip it under their tongue or in their cheek, and it dissolves while they fill out the paperwork confirming they did receive their dose. At the end of this, it is mandatory that I check under their tongue to make sure they are not saving the film and take the trash to make sure there is no way they save any part of the film. I have had repeat patients come back after thinking they have beat their addiction. I have had a mother break down in the pharmacy while thanking us for trying to help her son beat his addiction, even though he overdosed and died the week before. Then, there are the successes that seem few and far between and that make it worth it, but this epidemic is only getting worse.
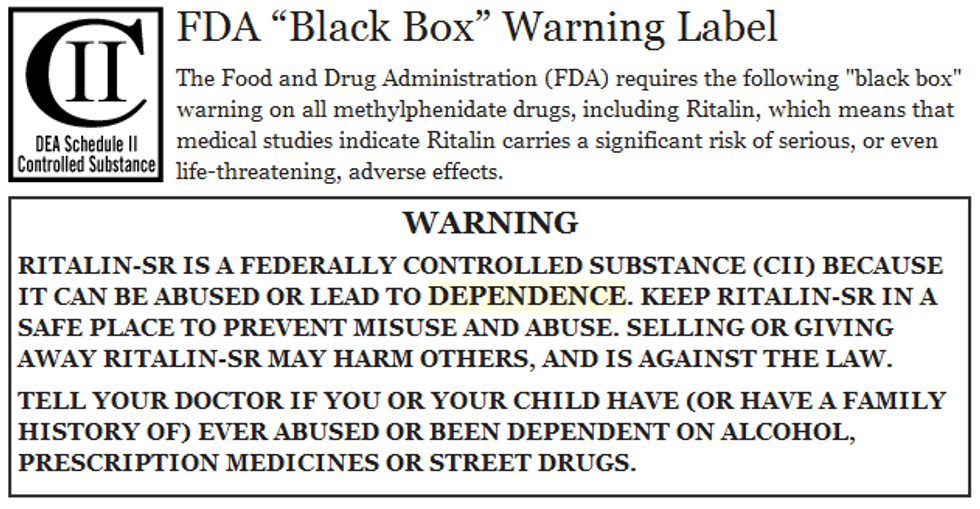
There are days where I count out up to 240 pain pills for a single patient as a one-month supply. There are times where these are terminally ill patients and other times its patients with chronic pain. The warning that goes along with these medications is currently minimal. This week the FDA announced that it will require common opioid pain medications, like morphine and oxycodone, to carry a black box warning. This is the strongest warning the FDA can issue in regards to medications. The warning will caution users of addiction, abuse, and overdose. The thought process is that this warning will make patients more aware of the risks of taking the medication and hopefully the prescriber will think twice about prescribing medications.
This is the black box warning currently used for Ritalin, which is an ADHD medication.
Oftentimes for long-term pain, prescribers jump right to opioid medications instead of trying something less severe for the pain or even trying physical therapy. There are times where people get injured, they throw out their back or tweak a knee, but is something as severe as a narcotic the first treatment option? After surgery for short periods of time like a week or two, opioids can be helpful. For months and months of treatment in a patient who is not terminally ill, it can lead to addiction problems very quickly. Patients don't understand that the medication they are taking will most likely cause withdrawal symptoms once they quit taking the medication. They don't understand that they need to ween off of the medication in attempts to make those withdrawal symptoms more mild. Patients don't understand how addictive these medications can be and how quickly the problem arises. These medications hit the same receptors as heroin. If you viewed your Norco or oxycodone as heroin, would you still take as many pills? I know this all sounds extreme, but taking it for a week or two isn't too addictive. You have friends and family hopefully supporting you through a short-term procedure and oftentimes people don't even finish the medications prescribed. This is how we hope things go, but more often than ever before, this isn't how the process goes.
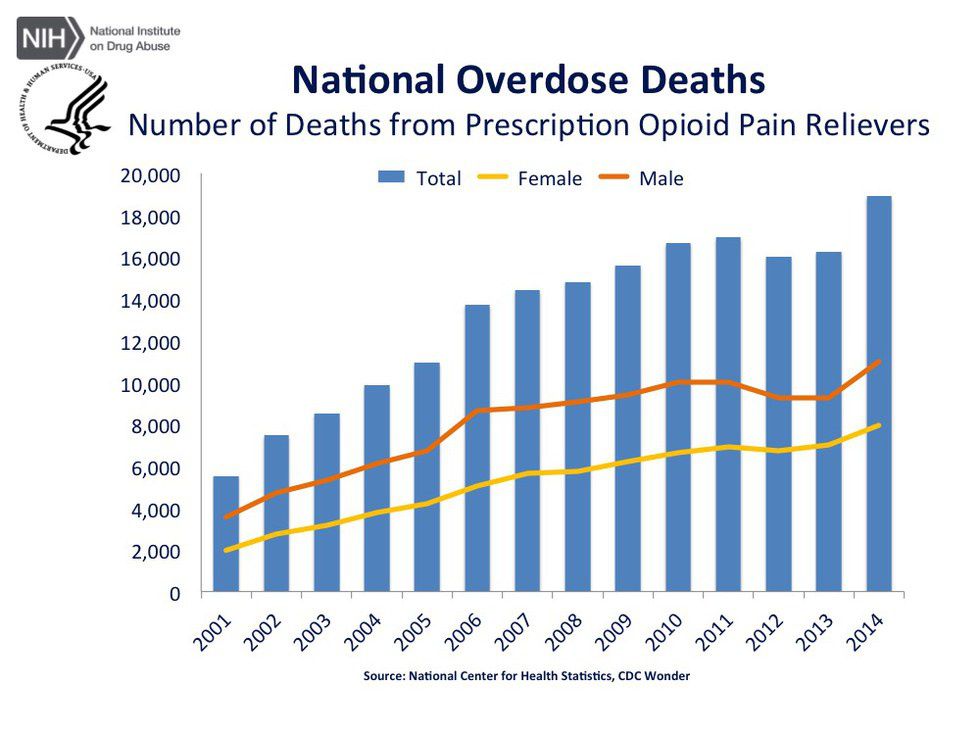
So here’s the question, will adding a label really make all that difference? Most people are aware of the risks that go along with taking an opioid and doctors are aware of the side effects. What does adding a label to the box do? Hopefully a lot. The FDA has taken a step towards recognizing that this problem is growing at a terrifying rate all across the country. The hope is that the rest of the country recognizes this issue and gets on board with decreasing prescribing and understanding the risks when taking the medication. The death rate is too high to continue at the rate we are.