Each year, around 13,000 United States citizens die from cancerous brain tumors. Not only are brain tumors known to be the most aggressive form of all cancers, they are one of the leading causes of cancer related death. The nature of this cancer has caused extensive inquiry into how to remove the tumor without causing damage to the brain, and how to keep it from returning. After a wide-range of research, with many different scientists, and over the course of many failed attempts, the Preston Robert Tisch Brain Tumor Center at Duke may have found a solution.
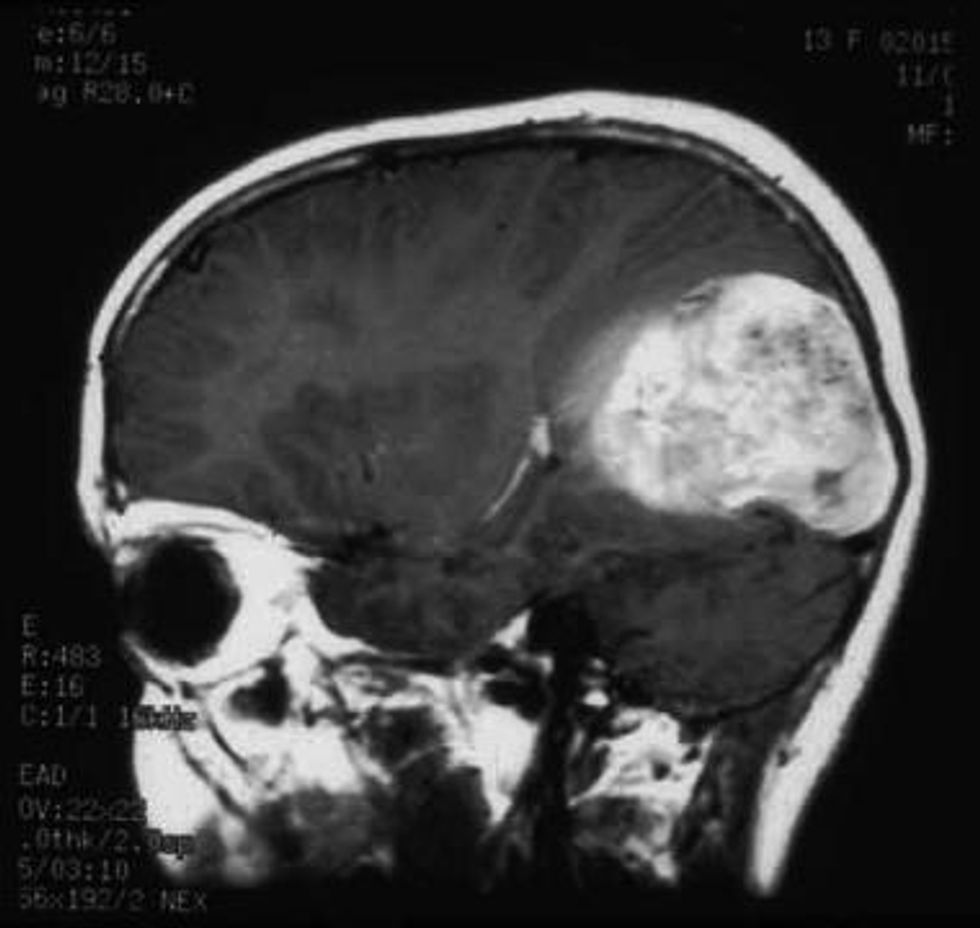
A tumor of this sort is most commonly known as glioblastoma. This cancer can be located anywhere in the central nervous system, but it is typically found in the hemispheres of the brain. Even though glioblastoma does not typically spread to other sections of the human body, it is known to be one of the most aggressive malignant tumors. This means that the cancerous cells reproduce at an extremely fast rate, making the cancer hard to control, and deadly. Also, there are many different types of cells in these tumors, making it difficult to target each of the components of brain cancer in one type of treatment. Three of these types of cells are blood vessels, calcium deposits, and cystic minerals. It is commonly known that when one is diagnosed with glioblastoma, that person is receiving a death sentence. An adult with this type of cancer typically survives around two to three years, but only if the tumor is found in the early stages and can be treated. However, if the patient is under the age of forty the chance of survival is higher than that of an older patient. Those patients in the later stages of their cancer are typically projected to live fourteen months after diagnosis.
An image depicting a very large Glioblastoma Tumor in the caudal portion of the brain.
Because of glioblastoma’s aggressive tendencies, it generally becomes very hard to cure. Once the tumor has been removed, it often comes back within a short amount of time, and it grows even faster than before. Therefore, it is common to treat glioblastoma with the aim of prolonging the inevitable. One of the first concerns with this form of cancer is to release the pressure within the brain to increase the comfort of the patient. Then, often times, the individual will go through a series of surgeries in order to remove the tumor. This tumor is especially hard to remove because of the branch-like nature that it possesses. Therefore, surgeons recurrently find that they are unable to remove the entire tumor for fear of harming the cerebral cortex.
A little over twenty years ago, scientists realized that the treatments offered for glioblastoma were not nearly as aggressive as the beast that they were facing. Research began promptly in an effort to find a faster way to eradicate the tumor completely. Scientists found that cancers have a protection around the tumor that makes them invisible to the immune system. It was decided that injecting a particle into the tumor (i.e. a virus) that breaks down this protection was necessary in the road to treating glioblastoma.
To fight cancer, a virus called oncolytic is required to target the cells and cause an infection. An oncolytic virus works by infecting and killing cancer cells. In turn, this virus will kill the the tumor and hopefully remove it all together. In research, scientists found that they could take the genetic code of the Poliovirus, remove the piece of it that causes the infectious disease and replace it with a piece of genetic information from a common cold virus. In doing this, they could ensure that the patient would not be infected with the actual Poliovirus. Instead, the toxins remove the protection around the tumor that makes it invisible to the immune system. Then, the glioblastoma patient’s body becomes alert to the tumor and attacks it as it should have all along. This genetically engineered form has now been renamed as PVS-RIPO.
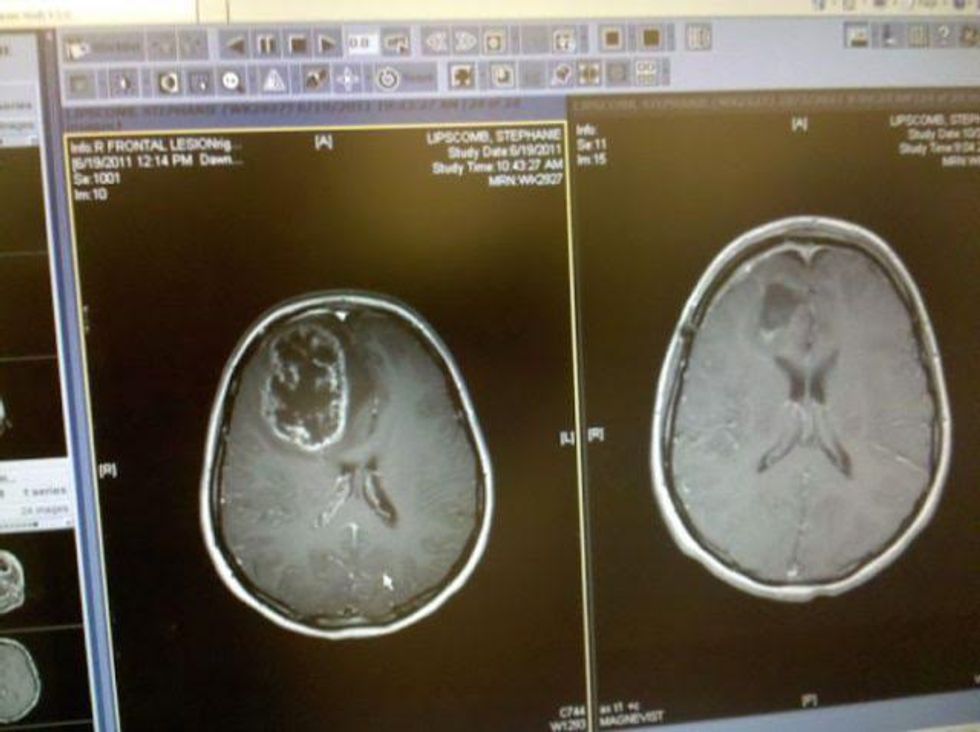
One very positive and heartwarming story gives hope to the theory of this breakthrough. A young woman; Stephanie received her diagnosis of glioblastoma in 2011 at the age of 20. After having ninety-eight percent of her tumor removed through surgery, and undergoing radiation, and chemotherapy, Stephanie’s glioblastoma was back and growing again less than a year later. She then decided to be the first patient to undergo the PVS-RIPO therapy, feeling as though she had nothing to lose. Dr. Henry Friedman —a neurologist at the Preston Robert Tisch Brain Tumor Center at Duke — spoke of Stephanie’s chances with this treatment. He said, “In point of fact, we didn't know what the polio was gonna do. We thought the polio virus might help her. We had no idea what it would do in the long haul. It was a crap shoot. It's roll the dice and hope that you're gonna get an answer that is coming up sevens and not coming up snake eyes.” In the following MRI sessions, Stephanie’s tumor showed swelling, but was without growth, gaining hope for the treatment’s effectiveness. For twenty-one months, the glioblastoma tumor shrank in size until it was gone, leaving only a small hole from her previous surgery. Three years after the infusion of the PVS-RIPO, an MRI depicted a miracle for those diagnosed with the most aggressive of malignant tumors. Stephanie’s brain was glioblastoma free.
Before (left) and after (right) imaging of Stephanie's glioblastoma tumor and then being cancer free.
This newly discovered treatment is a promising new step in the fight against cancer. Since this time the FDA has given this possible cure the designation of "Breakthrough therapy". It is hoped that through this route, not only will glioblastoma victims will be able to receive a much more effective form of treatment for their tumor, but other cancer patients can begin to be tested to see how effective PVS-RIPO will be on their tumors as well. With a finding this great, there is a new found hope for those who are living with malignant tumors. Glioblastoma no longer connotes a death sentence, but rather faith in a cure.